Chemo-Therapies for Breast Cancer
New chemo-therapies are rarely available, in this article we want to look at the treatment options of new and “old”, better, established breast cancer therapies. Breast cancer is the most common cancer in women, every 8th (~70000/a in Germany) suffers from it. The treatment of breast cancer depends on various factors, such as the stage, type and aggressiveness of the tumor. Chemotherapy plays an important role, which aims to kill cancer cells throughout the body or slow their growth. In this article, some questions about chemotherapy for breast cancer are answered.
We generally recommend accompanying and controlling the therapy with maintrac (cell count measurements).
What chemo-therapies are available for breast cancer?
Chemotherapy for breast cancer consists of administering drugs that are either given as tablets or as infusion. The drugs can be used individually or in combination. The choice of chemotherapy depends on various factors, such as age, general condition, hormone status, HER2 status (receptor on tumor cell surfaces) and risk of recurrence.
There are different types of chemo-therapies that can be used for breast cancer. Unfortunately, they are often unspecific and also attack healthy cells in the body and thus cause side effects.
Anthracycline-containing chemotherapy:
This chemotherapy contains drugs such as doxorubicin or epirubicin, which belong to the anthracyclines. Such drugs work by damaging the DNA of cancer cells and thus preventing their growth and division. Anthracycline-containing chemo therapies are very effective, but can also have serious side effects, such as heart damage or leukemia.
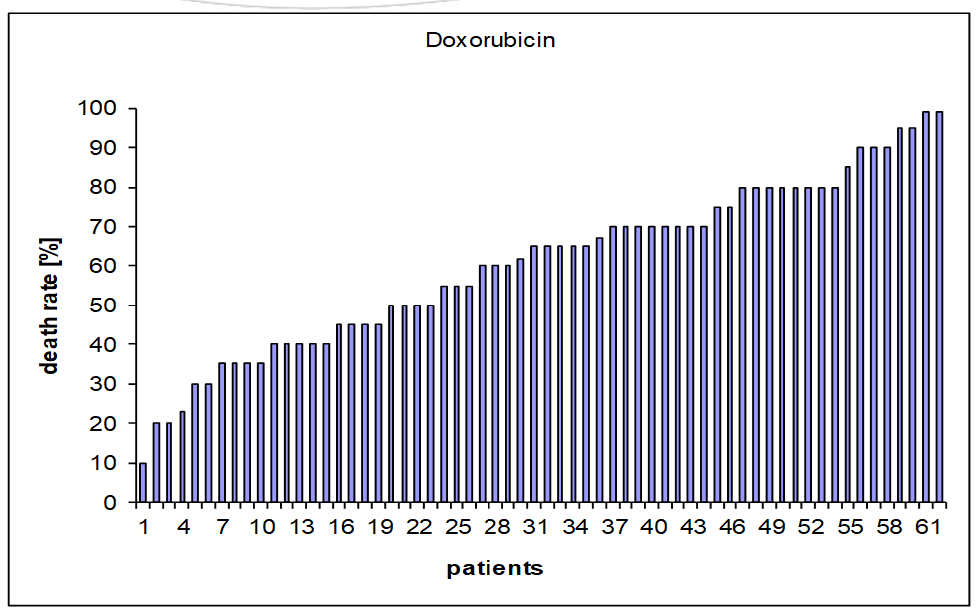
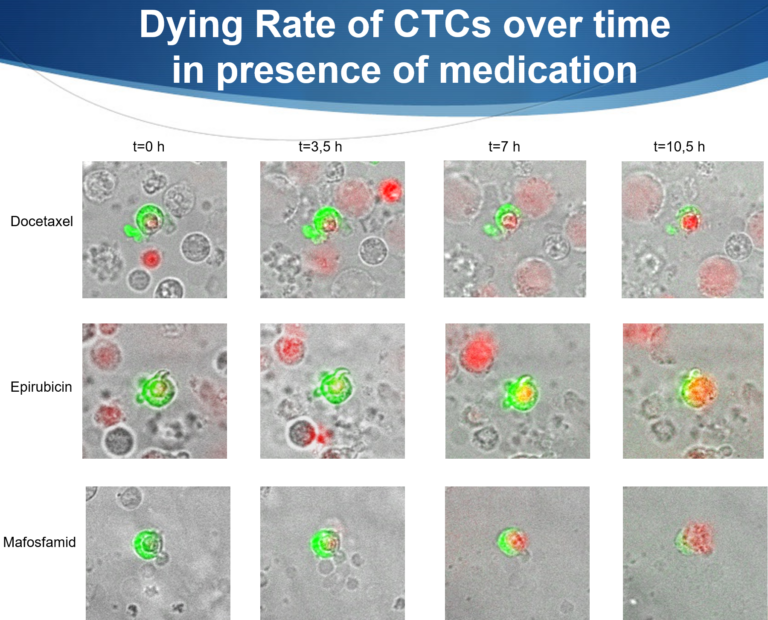
In this graph, the results of 62 patients are shown and the effect of doxorubicin on their circulating tumor cells (CTCs) was investigated. In 39 patients, a killing rate of CTCs of > 50% was measured and in 23 patients, a killing rate of <50% was measured. Therefore, it would be important to measure the effectiveness of the chemotherapeutic agents on the CTCs present in one’s own blood before chemo-therapies in order to receive a truly individualized therapy. Anything that kills more than 50% of the cells is defined as effective.
Taxan-containing chemo-therapies:
This chemotherapy contains drugs such as paclitaxel or docetaxel, which belong to the taxanes. These drugs work by disrupting the cytoskeleton of cancer cells and thus preventing their movement and division. Taxane-containing chemotherapies are also very effective, but can also have side effects, such as nerve damage or hair loss.
Platinum-containing chemotherapy:
This chemotherapy contains drugs such as cisplatin or carboplatin, which belong to the platinum compounds. These drugs work by cross-linking the DNA of cancer cells and thus preventing their repair and division. Platinum-containing chemo-therapies are mainly used in patients with triple-negative breast cancer, i.e. in patients whose tumors do not have hormone receptors or HER2 receptors.
Capecitabine:
This is a drug that is taken as a tablet and is converted in the body to another active ingredient called 5-fluorouracil. This active ingredient works by inhibiting the formation of DNA building blocks in cancer cells and thus preventing their growth and division. Capecitabine is mainly used in patients with metastatic breast cancer, i.e. in patients whose tumor has spread to other organs.
Cyclophosphamide:
This is a drug that is administered either as a tablet or as an infusion. This drug works by damaging the DNA of cancer cells and thus preventing their growth and division. Cyclophosphamide is often used in combination with other drugs.
Tukysa (Tucatinib)
In March 2021, a new chemotherapy in tablet form came on the market, which can be used for HER2-positive breast cancer and also metastatic breast cancer. It is a tyrosine kinase inhibitor that is combined with trastuzumab and capecitabine.
Tukysa application
Tucatinib is available as tablets in two dosages (50 and 150 mg tucatinib). The recommended dose is 300 mg tucatinib twice daily (two tablets with 150 mg tucatinib each). The treatment is stopped when the cancer progresses or too severe side effects occur.
Other treatment alternatives
For women with (HER2)-positive locally advanced or metastatic breast cancer who have previously received at least two HER2-targeted treatments, lapatinib in combination with capecitabine may be considered. Certain patients may also receive lapatinib in combination with trastuzumab.
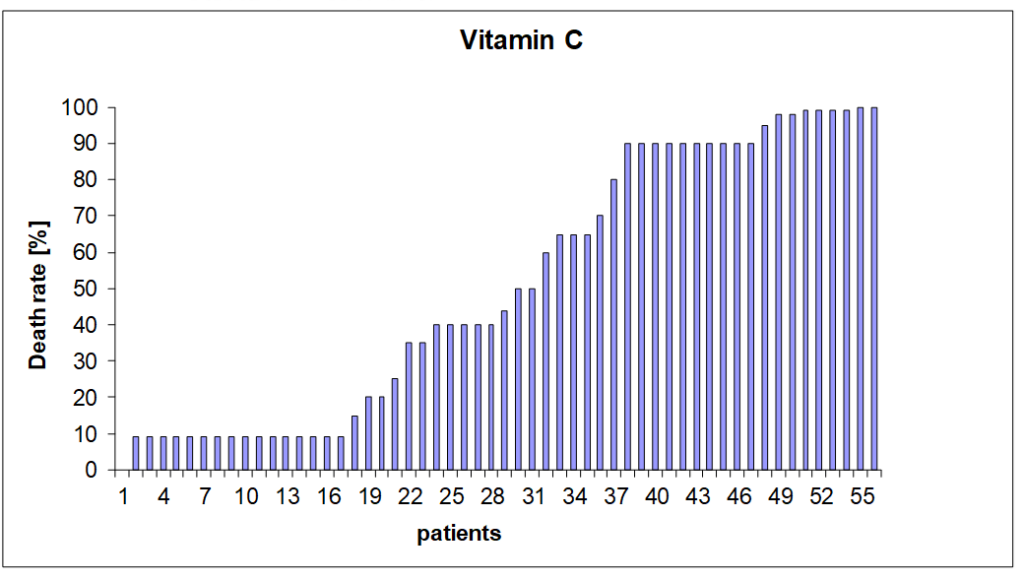
Often a high-dose vitamin C therapy is recommended. Our results from the laboratory show that 25 of these 52 patients would have benefited, but in 31 patients hardly any effect was to be expected, assuming that 50% killing rate is considered a success.
What is the difference between neoadjuvant and adjuvant chemo-therapies?
Neoadjuvant therapy is a treatment that is performed before surgery. The goal of this therapy is to shrink or destroy the tumor to allow for a better surgery or a breast-conserving surgery. Neoadjuvant therapy can consist of chemotherapy alone or in combination with a targeted therapy. It should be noted that although the tumor often shrinks, there is usually a remnant that is then surgically removed. Through this shrinking process, tumor cells can be flushed into the bloodstream and remain there for years. As long as they are not stem cells, the risk of tumor recurrence is very low, but if there are stem cells among them, there is a higher risk of recurrence. Therefore, the recommendation here is to regularly monitor the tumor cell count (CTCs) with maintrac after therapy.
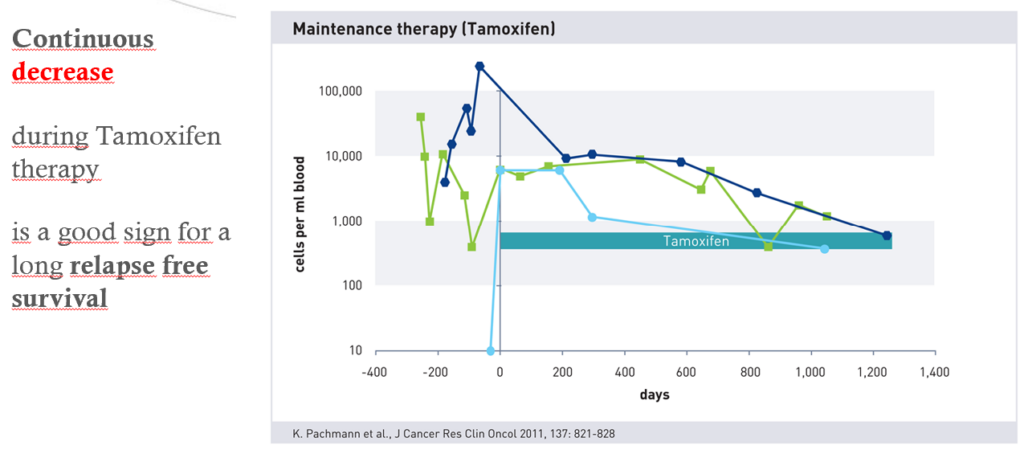
Neoadjuvant therapy from day -300 to 0. Typical zigzag curve. CTCs are scattered into the blood and are also killed. In the following days from 0 to 1300, a decrease in cell count is observed, which is synonymous with a good prognosis in almost all cases
Adjuvant therapy is a treatment that is performed after surgery. The goal of this therapy is to reduce the risk of relapse by eliminating possible remaining cancer cells in the body. Adjuvant therapy can consist of chemo-therapies alone or in combination with hormone therapy or targeted therapy.
Also, depending on the situation, tumor cells can enter the bloodstream through surgery and accordingly lead to a higher risk of tumor recurrence. Here too, monitoring the tumor cell count using maintrac is recommended.
When neoadjuvant chemo-therapies for breast cancer?
Neoadjuvant chemotherapy for breast cancer is mainly used in patients with HER2-positive or triple-negative breast cancer, as these tumor types are particularly sensitive to chemotherapy. Neoadjuvant chemotherapy can also be used in patients with hormone receptor-positive breast cancer if the tumor is very large or multiple lymph nodes are affected.
The advantages of neoadjuvant chemotherapy are:
- It could facilitate or enable a breast-conserving surgery.
- It can check the effectiveness of chemo therapies by observing the response of the tumor.
- It can improve survival by preventing the spread of cancer cells.
The disadvantages of neoadjuvant chemotherapy are:
- It can delay or complicate surgery if the tumor does not shrink sufficiently or becomes inflamed.
- It can increase the side effects of chemotherapy by impairing wound healing or weakening the immune system.
- It can limit the choice of adjuvant therapy if the tumor cannot be completely removed or there is a high risk of relapse.
When adjuvant therapy for breast cancer?
The advantages of adjuvant therapy are:
- It can significantly reduce the risk of relapse by killing possible remaining cancer cells in the body.
- It can improve survival by reducing the risk of metastases in other organs.
- It can be individually tailored according to the risk profile and preferences of the patient.
The disadvantages of adjuvant therapy are:
- It can have side effects that can affect the quality of life, such as nausea, hair loss, menopausal symptoms or heart problems.
- It cannot guarantee that the cancer will not return, as not all cancer cells may respond to the therapy.
- It may require a long treatment duration that can last several months to years.
Which is the most agressive Chemotherapy?
There is no clear answer to the question of what is the most aggressive chemotherapy, as this depends on various factors, such as the tumor type, stage, general condition and side effects. In general, however, a chemotherapy is more aggressive the more drugs it contains, the higher the dose is and the shorter the intervals between cycles are.
Aggressive breast cancer therapy
The most aggressive form of breast cancer therapy is high-dose chemotherapy followed by autologous stem cell transplantation. This therapy is used in women who have locally advanced or metastatic breast cancer that does not respond to other treatments.
The high-dose chemotherapy is intended to kill all cancer cells in the body, but can also damage many healthy cells. Therefore, before the therapy, stem cells are taken from the blood or bone marrow of the patient and frozen. After chemotherapy, the stem cells are returned to the body to regenerate the blood-forming system.
High-dose chemotherapy is also associated with high risks and side effects. These include, among others:
- Infections
- Bleeding
- Nausea and vomiting
- Hair loss
- Infertility
- Organ damage
- Secondary tumors
High-dose chemotherapy is therefore a very stressful therapy that is only performed under strict conditions and in specialized centers.
“Mild” breast cancer therapy
The mildest form of breast cancer therapy is anti-hormone therapy, also called maintenance therapy. It is usually performed after chemotherapy or radiation therapy. This therapy is used in women who have a hormone receptor-positive breast cancer. This means that the cancer cells receive growth signals from the female hormones estrogen and progesterone. The maintenance therapy is supposed to block these signals or reduce the hormone production, in order to stop or slow down the cancer growth.
The anti-hormone therapy is relatively gentle and well tolerated compared to other therapies such as chemotherapy or radiation. Most common side effects are:
- Hot flashes
- Sweating
- Vaginal dryness
- Mood swings
- Joint pain
- Osteoporosis
maintrac as monitoring and control diagnostics
The anti-hormone therapy is therefore a long-term therapy that is usually taken for several years. But here too, monitoring the cell count using the maintrac method is advisable. It can also be started at any time with the tumor cell count measurement. If you decide to do so, you can also order a blood collection kit here on our partner site.
Conclusion regarding new chemo-therapies
Developing a new, breakthrough drug for cancer therapy is associated with immense costs (several 100 million €). In addition, each cancer is a completely individual disease and should be treated individually contrary to existing standards. Often, a drug targets a specific biochemical process in the cancer cell. Unfortunately, however, only a part of the cells actually have this biochemical process or worse, all cells, healthy and sick, have this target point, which can then lead to massive side effects.
With the new Tukysa, a new preparation has come onto the market, which can only bring an extension of life by a few weeks in combination and under certain conditions with other drugs.
We are happy to help. Get well soon!

Dr. Martin Burow, Biochemist